

Let’s discover the next breakthrough in lupus clinical research, TOGETHER
People with lupus should have faster, more equitable access to safe and effective therapies. We’re on a mission to advance lupus clinical research, and with your help, we can make it happen sooner.
Accelerating Progress for the Lupus Community
As the clinical research accelerator arm of Lupus Research Alliance, we partner with biopharmaceutical companies, clinical investigators, and community organizations to improve the clinical research process. Our efforts have one ultimate goal – ensuring the lupus community has more therapies that better address the unique ways lupus can affect individuals.
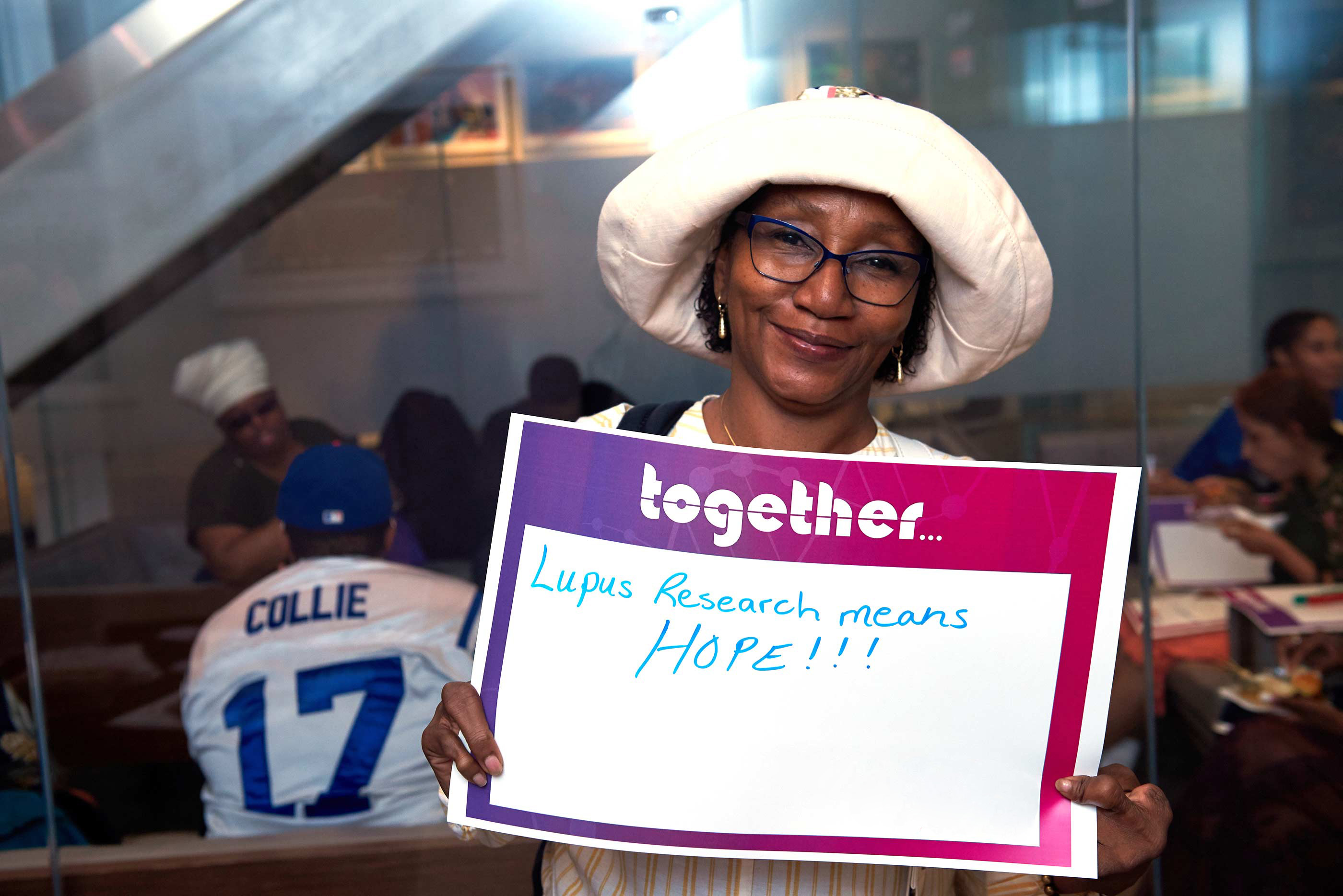
Driving Equitable and Inclusive Patient-Focused Research
Integrating the voices of patient peer advocates and lupus experts into every phase of the clinical research process is vital. To achieve this, we first need to eliminate the fundamental barriers preventing members of the lupus community from getting involved, particularly those from underrepresented groups. That’s why we’re spearheading several initiatives to improve access to clinical trials and increase participation rates among diverse communities, including Project CHANGE (Community-based Health Action Network to Generate trial participation and Eliminate disparities) and our PALS program (Patient Advocates for Lupus Studies).
Catalyzing Lupus Clinical Research
We help move research forward faster with our suite of medical and scientific consulting services for biopharmaceutical companies and our expansive, proprietary network of clinical trial sites at leading academic research centers throughout North America, known as our Lupus Clinical Investigators Network (LuCIN). Through LuCIN, we’re able to tap into the expertise of more than 200 experienced clinician-scientists focused on lupus research to help treat more than 25,000 people living with lupus.